Cortisone Injections.
Overview
What is cortisone?
Cortisone is the name used to describe a group of drugs commonly known as corticosteroids. The types of cortisone used at Melbourne Radiology Clinic include Celestone (Betamethasone), Kenacort (Triamcinolone) and Depot-Medrol (Methylprednisolone). Cortisone is used to treat pain in various parts of the body where inflammation is felt to be the cause of this pain. The reason why cortisone is effective in treating such pain is because it is a powerful anti-inflammatory. Cortisone is NOT an illegal steroid medication, such as those steroids used by some disqualified body builders and athletes
Why inject cortisone?
In regard to musculoskeletal problems, cortisone injections are performed in order to reduce or even eliminate pain associated with a variety of disorders, such as:
- Bursitis (most commonly subacromial and trochanteric bursitis)
- Arthritis (any joint may be injected, including joints of the spine)
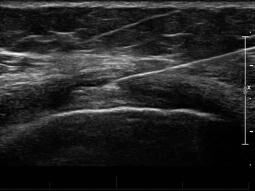
- Nerve pain (most commonly for sciatica and carpal tunnel syndrome)
- Tendinitis and Tenosynovitis (such as plantar fasciitis trigger finger, DeQuervain's tenosynovitis, Tennis and Golfer's elbow)
- Other miscellaneous conditions where inflammation is a contributor to the pain, for example frozen shoulder/adhesive capsulitis, Morton's neuroma, ganglion cyst injections and Dupuytren's contracture.
PROCEDURE
CORTISONE INJECTION
How is cortisone administered?
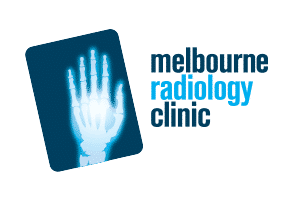
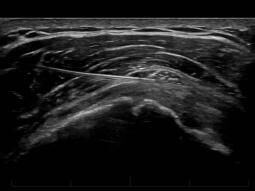
- The skin is prepared using an antiseptic agent.
- The needle is then guided into the relevant body part using medical imaging equipment, such as an ultrasound or Computed Tomography (CT) scanner. The guidance allows a high dose of cortisone to be accurately delivered into the area of suspected/proven pain without the side effects of taking cortisone tablets. This gives you the best chance of pain relief, as injections performed without guidance may not work due to incorrect placement of cortisone.
- The degree of discomfort during the procedure is generally mild as the needle used is fine and local anaesthetic is mixed in with cortisone. If only one pass is planned (meaning that the needle will only penetrate the skin once) then local anaesthetic is usually NOT injected into the skin. It is our experience that injecting local anaesthetic into the skin in a single pass procedure is actually more painful, as local anaesthetic stings a little prior to taking effect. Also, the needle used to inject the local anaesthetic results in similar discomfort as the needle delivering the cortisone. Local anaesthetic is only injected into the skin if more than one pass is made through the skin. Of course, if you wish for local anaesthetic to be injected despite our recommendation, we are happy to do this.
- A greater degree of discomfort may occur if:
– the underlying inflammation is severe
– the area to be injected is severely painful
– the needle tip requires to be repositioned several times in order to distribute the cortisone effectively
– a previous bad experience has resulted in a fear of needles, or there is a general anxiety/phobia of needles and other medical procedures.
In cases where a cyst, ganglion, bursa or joint is distended with fluid, the cortisone will be injected after an attempt to aspirate (remove) the fluid in order to improve comfort.
RISKS
As for all medical procedures, there are risk associated with the administration of any medication, including cortisone. The chances of cortisone providing you with the benefit of pain relief in most patients outweighs the risk of experiencing a side effect(s) (discussed below). The decision to inject cortisone is not taken lightly and is carefully made by your referring doctor and based on your signs, symptoms and past medical history, as well as the suspected diagnosis. Frequently, a trial injection is made where the diagnosis is not clear, however the body region that is to be injected is suspected of causing your pain.
The side effects and risks of a cortisone injection include:
Allergy to any of the substances utilised during the procedure, such as the cortisone, dressing, local anaesthetic or antiseptic. This is usually minor and self limiting.
The cortisone may result in palpitations, hot flushes, insomnia, and mild mood disturbance. This usually resolves within 24 hours and no treatment is necessary.
Infection is a rare but serious complication (<0.1%), especially if injected into a joint. Most infections take at least a day or two to manifest, so pain at the injection site after 48 hours is considered to be due to an infection until proven otherwise. Even if not definitively proven, you may be commenced on empirical antibiotic treatment.
Localised skin and subcutaneous fat atrophy (thinning resulting in dimpling).
Hypopigmentation (whitening of the skin) at the injection site. This most commonly happens in injections of the palm of the hand or sole of the foot.
Mild increase in blood sugar levels in diabetic patients for several days and may last up to a week.
Transient increase in pain at the injection site before the cortisone takes effect. Occasionally this may be severe, however usually lasts only 24–48 hours and is treated with a cold pack, paracetamol and anti-inflammatory medication. If this occurs and you are concerned, especially if the pain is not settling despite the above treatment, then please call contact your referring doctor so that they are able to examine, assess and manage you appropriately.
Cortisone injection administered directly into a tendon has been reported to weaken and damage the collagen fibers, thus carrying a risk of delayed rupture. For this reason, cortisone is only injected around the tissue surrounding a tendon and the tendon is rested for one week.
An extremely rare complication is avascular necrosis (bone death) which some doctors suspect may rarely occur when cortisone is injected into a joint, though this has not been proven
Remember that the side effects of cortisone that are commonly reported in the media, such as osteoporosis, weight gain, acne and diabetes only occur when taking cortisone tablets for at least several weeks (typically many months to years). These side effects do not occur with the careful use of cortisone injections.
FAQs
Are there any alternatives to a cortisone injection?
Of course there are. Since a cortisone injection is used for treating pain, it is an optional procedure. Other options should be discussed with you referring doctor and may include anti-inflammatory medications, exercise, physiotherapy and surgery to name a few. The role of our radiologist is to perform the procedure requested by your referring doctor and therefore ensure that the cortisone is injected safely and into the correct location.
How many cortisone injections are permitted?
There is no scientifically proven limit for cortisone injections, however as a general rule, three injections into the same body part are permitted over a twelve month period. Injections more frequent than this are felt to place the injected tissue at risk of softening/weakening, which may be an issue in a joint for example, as this may accelerate arthritis. Also, if you have failed to respond to a series of three injections, then it is probably time your condition was reassessed to find out if the diagnosis correct. Has your condition worsened and are other forms of treatment, such as surgery, more appropriate?
If you do require more than three injections in a year, then the risk of the injection must be carefully balanced against the benefits of pain relief. Your referring doctor or the doctor at Melbourne Radiology Clinic will be happy to discuss your condition and address any concerns that you may have.
Do you need to rest after a cortisone injection?
After a cortisone injection, it is strongly advised to rest the affected joint for 24 hours and refrain from doing strenuous activity or exercise for several days. Resting after the injection is vital to reduce inflammation effectively.
How long does a cortisone injection last?
Once administered, a cortisone injection begins to work almost immediately, although there are times when it may take five days to a few weeks for the full effect to be felt. Timing of relief varies depending on the severity of the inflammation or how long it has been present. Depending on the condition, a person may need more than one injection.
Results &
Follow-Up
One of Melbourne Radiology Clinic’s specialist radiologists, a medical doctor specialising in the interpretation of medical images for the purposes of providing a diagnosis, will then review the images and provide a formal written report. If medically urgent, or you have an appointment immediately after the scan to be seen by your doctor or health care provider, Melbourne Radiology Clinic will have your results ready without delay. Otherwise, the report will be received by your doctor or health care provider within the next 24 hours.
Please ensure that you make a follow up appointment with your referring doctor or health care provider to discuss your results.
Your referring doctor or health care provider is the most appropriate person to explain to you the results of the scans and for this reason, we do not release the results directly to you.