Nerves in the body pass through points of anatomic constriction, where they are bounded by rigid tissue. These often serve as sites of compression which may result in symptoms of tingling, numbness and muscle weakness.
Alternatively, these nerves may also be compressed by cysts and other types of masses, or a nerve may not function properly due to trauma or inflammation.
Injection of cortisone around the nerve sheath may suppress any inflammatory effect of the condition causing a patient's symptoms.
Even though the injection may not result in permanent relief of pain, prolonged relief may be achieved, so much so that surgery may be delayed. Further to this, even though the pain relief obtained from an injection may be transient, it nevertheless is a worthwhile procedure, as a good response to a cortisone injection is a reliable predictor of which patients will likely respond to surgery.
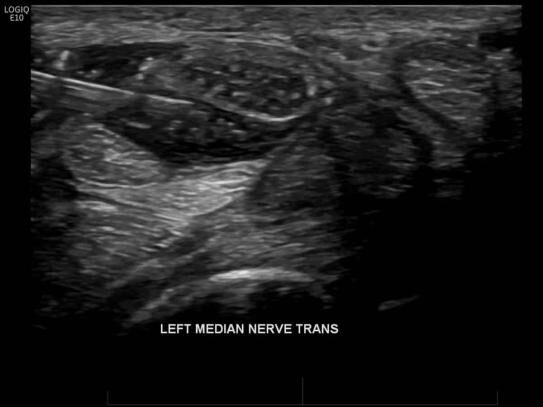
The most commonly injected nerve is the median nerve, which is classically compressed at the level of the carpal tunnel. This is commonly referred to as carpal tunnel syndrome.
Types of nerve blocks.
Nerve blocks performed include:
- Stellate ganglion blocks
- Lumbar sympathetic plexus block/chemical sympathectomy
- Brachial and lumbar plexus blocks
- Median nerve blocks (Carpal tunnel syndrome)
- Lateral femoral cutaneous nerve block for meralgia paraesthetica
- Nerve entrapment syndromes
- Occipital neuralgia (greater occipital nerve block)
- Post herpetic neuralgia
- Pudendal nerve block
Pudendal nerve block.
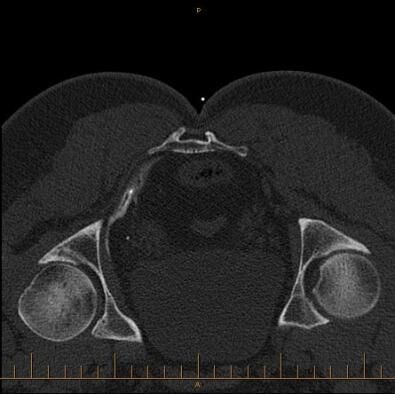
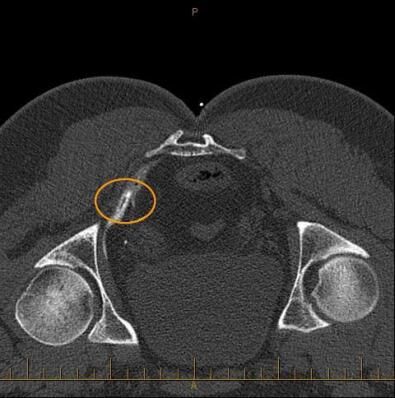
In the images shown, CT guided injection, following removal of needle demonstrates contrast around the pudendal nerve within the pudendal canal. This confirms needle placement and thus correct delivery of cortisone and local anaesthetic. Pudendal nerve blocks are used to treat long standing severe pelvic, anorectal and genital pain, the latter known as vulvodynia in females.
References:
- Fanucci E, Manenti G, Ursone A, Fusco N, Mylonakou I, D’Urso S, Simonetti G. Role of interventional radiology in pudendal neuralgia: a description of techniques and review of the literature. Radiol Med 14(3):425-36, 2009
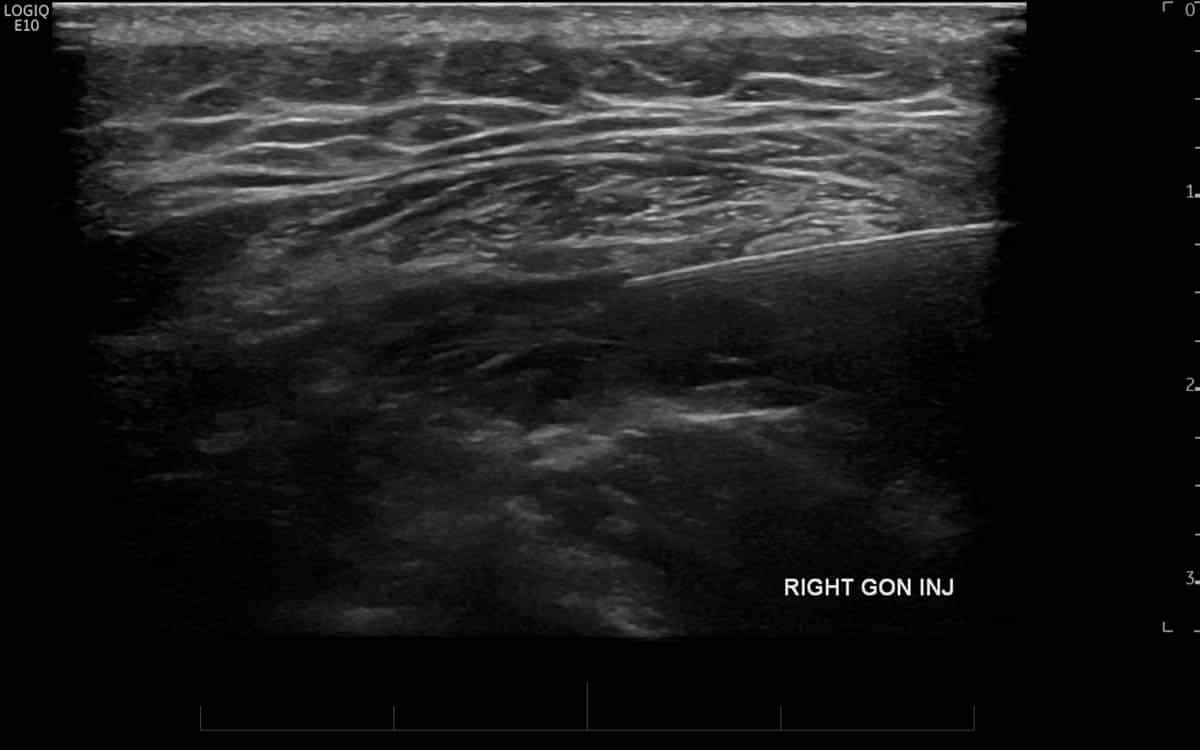
Occipital neuralgia
(greater occipital nerve block).
Irritation and inflammation of the greater occipital nerve, a nerve that arises from the upper cervical spine and supplies the skin and soft tissues of the base of the skull (also known as the occiput, or occipital region) is a common cause of headaches within this region. This most frequently occurs due to degeneration and inflammation of the facet joints immediately deep to the greater occipital nerve secondarily affecting the manner in which the way the nerve transmits pain and when becomes symptomatic, is known as the clinicial syndrome of Greater occipital neuralgia.
Injecting the nerve with cortisone under either CT or ultrasound guidance is an effective treatment option for this condition and is more effective than injecting “blind”, that is to say, without imaging guidance [1].
References:
- Jae Hang Shim, So Young Ko, Mi Rang Bang, et al. Ulltrasound-guided greater occipital nerve block for patients with occipital headache and short term follow up. Korean J Anesthesiol 61(1): 50–54, 20011
Further Information.
Referring doctors are welcome to discuss with our radiologists the imaging and interventional radiology needs of their patients and whether a nerve block is suitable for their patient’s medical condition.
Patient Guides.
Naturally as the human body contains an enormous amount of nerves that are amenable to injection, individual fact sheets with specific information pertaining to each separate nerve is beyond the scope of this website. Therefore, each nerve block injection procedure unique to your case will be discussed between you and your referring doctor as well as our radiologist. CT or ultrasound will be used to guide the needle accurately and safely.